HIV-Transmission under HAART – Lancet study rather supports „Swiss Statement“ than challenging it !
Hier Klicken für Deutsche Version
In tomorrow’s issue of the Lancet, Australian authors present a mathematical model to calculate the HIV-transmission risk under a HIV therapy. At the first sight it seems as if the calculations question the Swiss statement on HIV infectivity under HAART. However, an exact consideration of the paper rather strengthens the Swiss statement, as the authors of the editorial suggest.
The "Swiss Statement" was an information to Swiss physicians that the Swiss Commission on AIDS-related issues presented issued in January 2008. It said that physicians could inform their patients that the sexual transmission risk to the partner is negligibly low if three conditions were met:
- HIV-infected patient is under a physician controlled antiretroviral therapy with excellent adherence
- Blood viral load has constistently been undetectable (<40cp/ml) for more than 6 months
- no sexually transmitted diseases are present in neither of the partners
The statement also made clear, that it is only the HIV negative partner who can decide for himself whether he/she wants to stop using condoms with the treated partner.
The authors of the Lancet article from the 26.7.08 (David P Wilson, Matthew G Law, Adnrew E Grulich, David A Cooper, John M Kaldor) analyse potential consequences on new HIV infections if the Swiss statement would be followed. In their mathematical model the authors use the known Rakai partner study as their basis (Quinn et al, NEJM 2000). This work has shown that the risk of transmission is dependent on the virus load in the blood. In this population of approx. 450 HIV-discordant couples the HIV-transmission risk was doubled (x2.45) with every 10-fold rise of viral load in the blood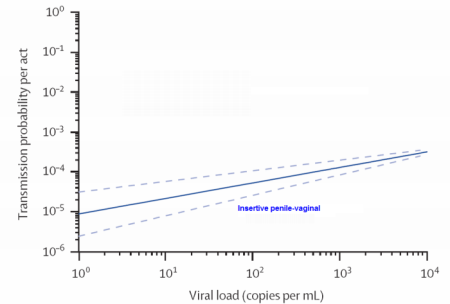
Simple mathemathical model used
The authors used this factor and computed a linear model in which the transmission risk was extrapolated for very small values of viral load. The transmission risk per sex act was therefore calculated for values of blood viral load around 10 cop/ml. The linear approximation is shown in the figure at right (click on figure for enlarged view). By definition, the transmission risk of such a log-log curve can never be zero. In other words, the authors refuse the existence of a threshhold level, below which no transmission would occur.
Estimation of the transmission risk by anal sex
In the Rakay study, only heterosexual couples were included. To calculate the per contact risk of anal sex among men having sex with men (MSM) for very low viral load values, the authors took the linear model (above) and elevated this curve by the mean difference in transmission risks among heterosexual couples and MSM (factor 20). This "parallel movement" of the risk increases the threshhold problem mentionned above. With this extrapolation, the authors receive highly unplausible values: Based on this calculation, the risk of transmission in one receptive anal contact with a man having only 10 viral copies per ml of blood (i.e. 5 viruses!) would be 1 in 6000. Such a risk estimate is hardly plausible. In the Swiss HIV cohort study (and presumably elsewhere, too) almost 20% of the patients do not use condoms consistently with their steady HIV-negative partner (Panozzo et al).
Reality differs!
In fact, such a high risk of transmission under HAART would be difficult to oversee. After all these years of HAART, we would expect to have documented several occasions of HIV transmision. Many experts as myself have been searching for such unusual cases over many years. As the Swiss Commission clearly stated: the risk is not zero (can never be assertained) but it must be in the range of our normal daily risks and this statement was restricted to situations very specific situations (see conditions above).
Most important risk factor for sexual transmission: Sexually transmitted infections
The mathematical Model presented in the LANCET did not consider one key aspect of the Swiss statement: The most important factor (beside blood viral laod) that increases transmission risk, namely sexually transmitted diseases (STD), namley syphilis, gonorrhea, trichomoniasis and herpes. Such STDs have certainly fueld transmission in the Rakai-Study as well. We know that genital viral concentration can increase 10-fold in the situation. In part, the increased average transmission risk among MSM are a result of the incresed incidence of STDs in this population. The Swiss statement has emphasized the absence of STDs, therefore a caclutlation including the risk in the presence of STDs cannot falsify the Swiss statement.
In summary, it seems obvious, that all the mentioned biases of the mathematical model will increase the risk estimate for HIV transmission under HAART.
Swiss Statement: Distinction, not absolution!
The Swiss Statement was widely misinterpreted by many people who have never read the original paper. The statement is not an "absolution" for HIV-positive indivuduals under fully suppressive HAART. Rather, the statement made a clear distintion of a subgroup of individuals with very limited risk to transmit the virus. Prior to our statement, many physicians have talked in private to their patients and informed them about a the limited risk of transmission under HAART. However, the informations were not openly communicated and to our best knowledge were seldom stressing the importance of the absence of STDs. One goal of the EKAF statement was to stress the importance of STDs and perfect adherence in communications regarding the very low risk of HIV-transmission under HAART. At least in Switzerland, this goal was clearly achieved and the message was well accepted.
The Australian study supports the Swiss statement
In fact, the data presented by Wilson et al. acutally support the Swiss statement as the editorialists (Garnett & Gazzard) conclude. In their commentary, Garnett a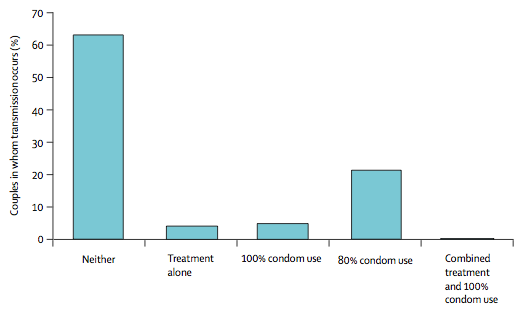 nd Gazzard have calculated per couple transmission risks based on the assumptions included in the Wilson paper (after 100 sexual episodes). Wilson et al. also included an estimate of the effectiveness of condoms. Using these figures, Garnett et Gazzard found that 100% condom use in the absence of HAART was as risky (or even riskier) than having sex without a condom on a fully suppressive HAART (see figure, click on figure to enlarge). In fact, this was exactly what the Swiss statement said: The residual risk of transmission on HAART without a condom was in the same range than having sex without condom in the absence of treatment. Thus, the Australian authors assumptions acutally confirmed the Swiss statement.
nd Gazzard have calculated per couple transmission risks based on the assumptions included in the Wilson paper (after 100 sexual episodes). Wilson et al. also included an estimate of the effectiveness of condoms. Using these figures, Garnett et Gazzard found that 100% condom use in the absence of HAART was as risky (or even riskier) than having sex without a condom on a fully suppressive HAART (see figure, click on figure to enlarge). In fact, this was exactly what the Swiss statement said: The residual risk of transmission on HAART without a condom was in the same range than having sex without condom in the absence of treatment. Thus, the Australian authors assumptions acutally confirmed the Swiss statement.
Responsible patients are able to decide for themselves
The Swiss statement never assumed a zero risk under fully suppressed HAART but rather stated, that the risk is in the range of other risks in daily life. In fact, the risk of transmission during condom protected sex in the absence of treatment is not zero either, nor is the risk of oral sex (without ejaculation). Nevertheless, oral sex and condom use are widely accepted methods of safer sex.
Other risks of daily life are also illustrative: Among 200’000 Swiss alpinists that spend a weekend in the alps, ten loose their lives every year in an avelange. This risk (1:20’000) is socially accpeted and regular insurances cover it without recourse. The Swiss HIV Experts considered it reasonalbe that an HIV-negative Parnter might be informed by the physician about the neglible risk. It was felt that the partners may decide for themselves how to deal with the final residual risk. This is comparable to the alpinist or to the partner who practices oral sex without condoms. They have all been adequately informed about their limited risk.
Other problems of the mathematical model
For the more experienced reader I would like to mention two other problems of the mathematical model by wilson et al. One is relates to the calculation of a cumulative risk (after 100 or 1000 sexual contacts). Epidemiological studies have told us, that the risk of transmission decreases over the duration of a partnershipt. To some extent, an aquired cell-mediated or mucosal immune defense might be responsible for this decline in transmission probability. Very little viral exposure might stimulate the immune defense rather than lead to full-blown infection. A biological fact that was not considered in the mathematical model, where each sexual contact is associated with the same risk. However, biological considereations would rather suggest that there is a threshhold for sexual transmission below which the development of an HIV specific immune response in the partner is more likely.
These biological observations might also play a role in the difference in transmission risk estimates between heterosexual couples and MSM. The higher estimate of transmission risk in MSM might in part also be a result of a higher proportion of parnterships with a shorter duration. In fact, two studies of female-to-male transmission after a single exposure in Kenia and Thailand found a transmission probability that was at least tenfold higher (3-8%) than in established partnerships and in the same range as for MSM. Thus, the risk estimates for MSM used by Wilson et al. might also be based on wrong assumptions.
Source: Wilson et al, Lancet 26.7.2008, 372:314-20
Editorial: Garnett & Gazzard, Lancet 26.7.2008, 372:271-2