Primary HIV infection (TEAM rounds)
What is primary HIV infection
Approximately 70% of patients who are infected with HIV will develop an acute, almost always febrile episode which is termed acute HIV infection. The syndrome of primary HIV infection (PHI) often manifests with rash and is often described as a “mononucleosis” like syndrome. In fact, mononucleosis is the most frequent misdiagnosis in patients with PHI. The major problem in the diagnosis of acute HIV infection is the fact that physicians fail to include acute HIV infection in the differential diagnosis. However, in some instances the physician dismisses the diagnosis of PHI based on a negative medical history. However, it has been shown that a sexual history is only suggestive in 50% of cases, while the other half of patients with PHI do not reveal their risk behavior until the laboratory diagnosis is made.
PHI is often accompanied by an STD
The first case presented in Geneva PHI occurred concomitantly with syphilis. Hearing loss was the leading symptom and it remains unclear whether this was a sign of secondary syphilis, HIV or both. While hearing loss was described as a symptom of syphilis in our textbooks, it is not known with HIV. However, PHI not rarely manifest with mild to severe forms of encephalitis and involvement of the inner ear is a plausible symptom of encephalitis. All the experts agreed that a treatment against both pathogens was warranted in this case. However, the case also illustrates a very important epidemiological aspect: Sexually transmitted diseases are clearly known to increase both susceptibility and infectivity for HIV. While most STDs (usually Chlamydia trach.) remain undiagnosed, PHI can lead to the diagnosis of an underlying sexually transmitted disease. Due to the obvious epidemiological consequences, contact tracing of patient with PHI or STDs should always be attempted if possible.
Diagnosis of PHI
Laboratory diagnosis is therefore the mainstay of the diagnosis of PHI. However, antibody screening is often negative in early cases of PHI. During this phase of the disease, antigen can almost always been detected at high levels in the blood of patients with PHI. The so called fourth generation HIV-screening tests will detect antibodies and viral antigen (p24) in the same test. The routine use of these tests has significantly improved the detection rate of HIV. However, since not all laboratories do use these tests on a routine basis, physicians need to inform their lab about their clinical suspicion of PHI. A more costly way to diagnose PHI would be with the use of HIV-RNA tests. However, in cases with clinical signs of PHI no study has so far shown an increased sensitivity of HIV-RNA versus p24-antigen.
Why is there any urgency in treating PHI
Patients with chronic infection will only be treated when some degree of immunodeficiency has occurred. Why should patients with acute HIV then be treated at all. The impetus to treat as early as possible originates in a number or immunological studies. 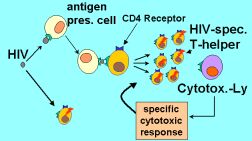 It is know clear that during acute HIV infection the virus predominantly infects not just activated T-helper cells but actually is infecting HIV-specific T-cells. HIV-specific CD4-T-cells are cells that are equipped with the appropriate antigen to recognize HIV-proteins. These cells are actively recruited by HIV-infected antigen presenting cells, proliferate and get activated. Since HIV infects predominantly activated cells, the HIV-specific T-cells are preferentially infected and exhausted during primary HIV-infection (see fig.) The theoretical concept of early treatment during PHI assumes that early treatment can preserve the HIV-specific immune response. However, in most instances, when treatment is interrupted, HIV will replicate and destroy HIV-specific targets similar to the situation during PHI. Some case reports – similar to the one presented here in Geneva (Paula) have acutally shown that some patients treated very early in HIV infection remain HIV-RNA negative after cessation of treatment. The GSK-sponsored QUEST study did evaluate whether preservation of the immune-response through active early treatment can be coupled with a stimulation of the immune response using a vaccine prior to the treatment discontinuation. The idea was that an immune response that is established prior to the cessation of the immune therapy might enable the immune system to fight HIV replication itself. So far, the QUEST study has not been able to demonstrate a marked change in the natural history of the disease. However, since we do not know whether the vaccination used in QUEST (the only one available when the study was planned) is able to mount a broad cellular immune response, the failure of QUEST does not falsify the prinicpal hypothesis.
It is know clear that during acute HIV infection the virus predominantly infects not just activated T-helper cells but actually is infecting HIV-specific T-cells. HIV-specific CD4-T-cells are cells that are equipped with the appropriate antigen to recognize HIV-proteins. These cells are actively recruited by HIV-infected antigen presenting cells, proliferate and get activated. Since HIV infects predominantly activated cells, the HIV-specific T-cells are preferentially infected and exhausted during primary HIV-infection (see fig.) The theoretical concept of early treatment during PHI assumes that early treatment can preserve the HIV-specific immune response. However, in most instances, when treatment is interrupted, HIV will replicate and destroy HIV-specific targets similar to the situation during PHI. Some case reports – similar to the one presented here in Geneva (Paula) have acutally shown that some patients treated very early in HIV infection remain HIV-RNA negative after cessation of treatment. The GSK-sponsored QUEST study did evaluate whether preservation of the immune-response through active early treatment can be coupled with a stimulation of the immune response using a vaccine prior to the treatment discontinuation. The idea was that an immune response that is established prior to the cessation of the immune therapy might enable the immune system to fight HIV replication itself. So far, the QUEST study has not been able to demonstrate a marked change in the natural history of the disease. However, since we do not know whether the vaccination used in QUEST (the only one available when the study was planned) is able to mount a broad cellular immune response, the failure of QUEST does not falsify the prinicpal hypothesis.
To treat or not ?
In summary, there is no evidence-based approach to the treatment of PHI. Nevertheless, many experts start treatment immediately when PHI is diagnosed. According to Joe Eron and other experts in this TEAM round, it is correct to start treatment since “it makes perfectly sense”. The hope is, that PHI-treatment can ultimately change the natural history of HIV infection. No guidelines exist about the duration of such treatment. Of course, treatment in this situation should only be maintained as long as no side effects occur.